The biggest difference between spinal blocks vs epidurals is their amount of pain relief: spinal blocks provide total pain relief, while epidurals provide partial pain relief. The reason for this difference is that the former is an anesthetic, while the latter is an analgesic—no sensation versus no pain.
But pain elimination comes with a total lack of feeling in the lower body, due to the blocking of spinal nerves.
Epidurals still allow for the pushing required of the second stage of labor, so spinal blocks are often used in conjunction with C-sections, though the amount of pain medication may need to be reduced to provide enough feeling for pushing.
The procedure that’s right for you will depend on the specifics of your birthing experience. Be ready for whatever comes by noting the pros and cons of both spinal blocks and epidurals below.
What is a Spinal Block?
A single dose of anesthesia into the fluid around the spinal cord. It’s also known as a saddle block, as it blocks sensation primarily from the pelvic floor, which is the muscle group most used during childbirth. Spinal blocks are not as popular as epidurals today. Only providing pain relief for two hours, many patients need repeat doses. Multiple injections into the spine are enough to make most opt for an epidural, which can even be administered using a dosage-capped patient-directed pain pump.
- Spinal block vs. spinal epidural: Is a spinal block the same as an epidural? The difference between these two similar terms is that the block is a one-time application of painkiller via needle, while the epidural permits continued applications via a catheter.
- Complex birth situations: A delivery that is happening very quickly, or one that requires forceps to help the baby along—these are just a few examples.
- Caesarian: When no pushing is required, a full block of sensation in the lower body becomes an option. Plus, patients don’t usually feel any pain, though some still report it or report better efficacy on one side of the body.
Advantages of a Spinal Block
If delivery is happening now, or if pain is anticipated to be short-term (2-4 hours), then a spinal block is a good option.
A spinal block is actually more of a versatile procedure than it gets credit for as just a pain relief tool. It’s helpful in creating break time to gather strength for impending delivery, and to keep mothers awake and aware during their C-section, so that they may experience the birth of their child. In fact, spinal blocks for C-sections are very commonly used.
- Complete pain relief
- Fast-acting
- Single injection
- No catheter
- No mental change
- Stay conscious during baby delivery during C-section
- Labor break to muster rally for delivery
- Safer than general anesthetic during intervention
Disadvantages of a Spinal Block
The possible spinal block side effects of a spinal block aren’t necessarily worth the short-term —although complete—cessation of pain.
- Only lasts 2-4 hours
- Single injection
- Low-grade headache more likely
- Difficulty urinating, itching, shivering, nausea
Possible Complications
Although rare, it’s important to be fully aware of any complications whenever undergoing a surgical procedure. Remember that many of these risks are carried with any surgery, such as infection, though when dealing with the spine, greater ramifications can result from complications.
- Infection: Many patients self-administer medication via injection, so it’s not just medical professionals who are at the risk of operator error with injections. The CDC maintains that proper safe injection practices can eliminate needle risks, such as contamination or transmission of a bloodborne disease.
- Broken needle: Needles do break at times, something every dentist has experienced or heard. The weak point of every needle is the hub, and some dentists even bend their needles, which has led to speculation that they break as a result.
- Hypothermia: Body temperature is considered hypothermic when it drops below 95°F. Excessive shivering, clumsiness, confusion, slowed speech, stumbling and slowed breathing are the primary symptoms. Patients who experience anesthesia often are in cold environments (operating rooms), under the influence of vasodilators which pull heat from the core, and wounds cause evaporation.
- Cardiac arrest: Anesthesia has been proven to be a contributing factor, or even a leading cause, in cardiac arrest, a small percentage of the time.
- Nerve injury: Nerves can be injured during injections, a common challenge faced by anesthesiologists. Most often the ulnar nerve is affected, and usually the discs of the spine that can shift (lumbar and cervical) are involved.
What does a spinal block feel like?
Perhaps the most important question of all—what does a spinal block feel like? Anything involving the spine and needles, particularly long ones, is likely to strike a nerve with patients.
An important note on pain with a spinal block: when it’s used outside of a C-section, sedation is administered. But because the baby can’t receive any sedation, mothers also can’t be sedated during a spinal block. The assumption many would make from this information is that you may feel pain during the procedure, potentially a heavy dose of it—otherwise, why would sedation be standard.
Pain
Generally, pain for a spinal block procedure refers to the insertion of the two needles: one to inject the anesthetics and one to guide the way to the spinal fluid. With sedatives and local injections, pain shouldn’t be an issue. Some patients still report it, but most get immediate relief from a shot of anesthetics into the dural sac of the cerebral column. Below is the difference between anesthesia and analgesia, to give more context on pain. Pain is also strongly subjective, with everyone having what appears to be varying tolerances and interpretations of pain.
- Anesthesia: loss of sensation
- Analgesia: loss of pain
The Procedure
You’ll lie down or on your side and arch your back, to enable easier insertion of the needles into your spinal area. Your lower back will be wiped with an antiseptic solution before your anesthesiologist selects a location. A fast-acting local anesthetic is injected, resulting in a small amount of pain similar to a bug bite. Once the area is completely numb, a thicker needle is guided into the spinal area by your anesthesiologist.
Technical Details
Here we’ll discuss spinal blocks in more technical detail, for those who want more than an overview.
- Anesthetics Used: Spinal blocks require local anesthetics, the most common of which is bupivacaine (marcaine). However cinchocaine, levobupivacaine, ropivacaine, procaine, tetracaine and the most well known, lidocaine, are also used in spinal blocks. These are the so-called ‘caine anesthetics’ derived from the original anesthetic, cocaine.
What is Recovery Like?
Fortunately, recovery for spinal blocks is short. You’ll recover feeling in your legs within 1-4 hours.
- Possible Long Term Headaches (Post Dural Puncture Headaches or PDPH): Usually when headaches are mentioned around spinal blocks, it gives the impression that these are short-term. But the piercing of the dura is a real risk with every spinal block. If this happens your headaches can last months, dissipating and returning, in a condition called Post Dural Puncture Headache, or PDPH. These headaches can also be long term side effects of a spinal block for C-sections.
The Spinal Block Advantage
A spinal block is a complete elimination of sensation in the area of the body required for a medical procedure. It is not like general anesthesia as it does not cause unconsciousness. However, it is a potent form of anesthetic. Every patient is different, with varying pain tolerances, health conditions, age-related challenges, so a spinal block that’s right for some is perhaps best administered as an epidural for others, according to the consultation of a medical professional.
Patients like spinal blocks because they are fast, completely effective, and only require one application. A catheter hanging out of your back during an entire pregnancy, for example, may not be desirable, particularly if lying on one side is a problem. When the pain of pregnancy is felt even with an epidural, patients opt for spinal blocks to completely eliminate pain.
What is an Epidural?
An epidural is a catheter fed into your spinal fluid, allowing for continuous administration of anesthetics. This is hugely important in first births, which can last from 12 to 18 hours. Spinal blocks, which only last for 1-2 hours, would have to be re-administered, wasting time, risking pain, and increasing the likelihood of infection.
The Epidural Process
Epidurals are most associated with birth, but they have many applications. Epidurals become an option as a birth pain solution when the cervix is dilated to a minimum of 4cm. But the epidural name only refers to using the epidural space of the spine to administer pain relief drugs. Where that relief is targeted is dependent on where a particular procedure is being performed; in a lung operation, for example, the chest cavity can be anesthetized.
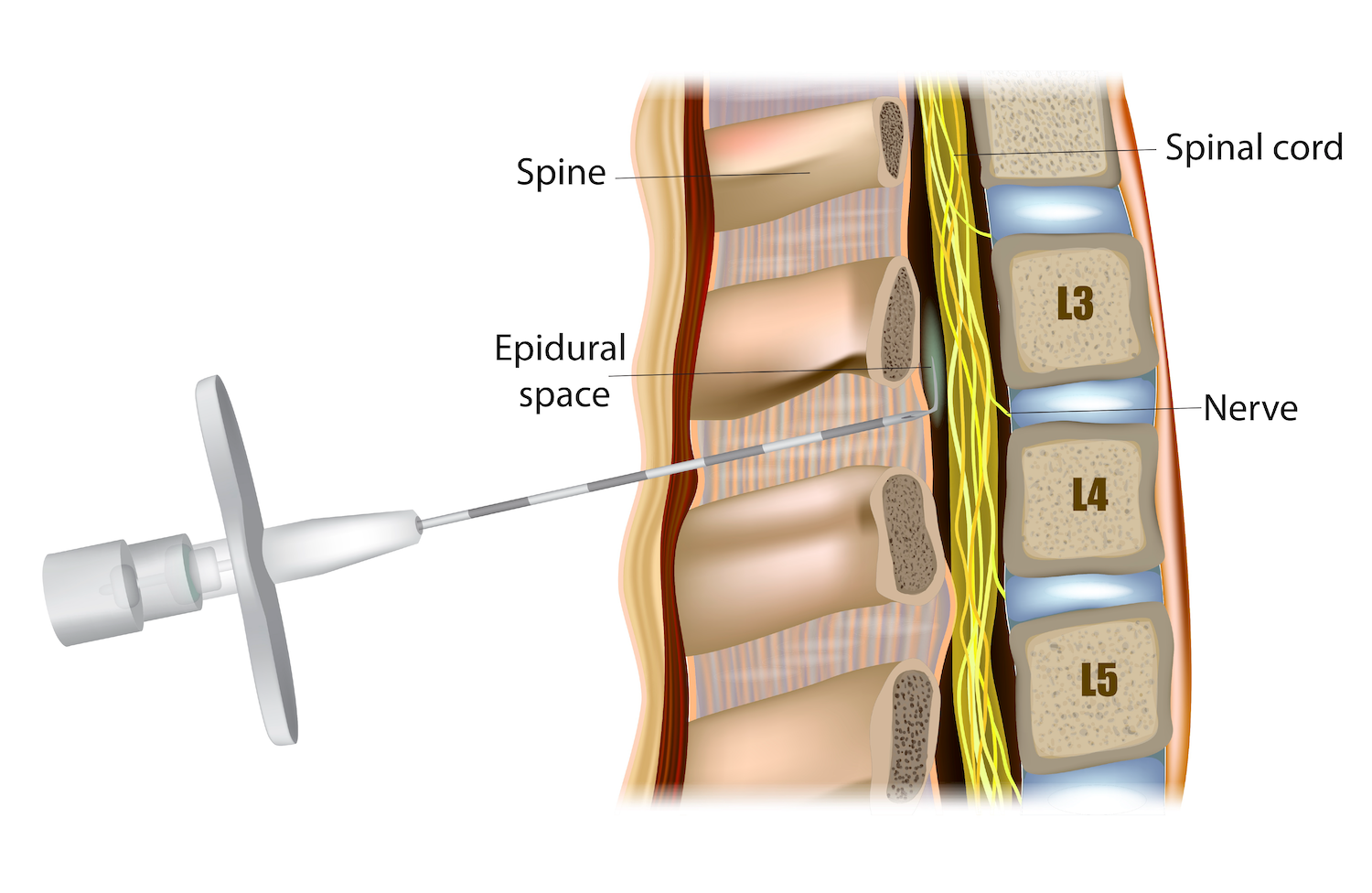
- Your anesthesiologist selects a location on your lower back and inserts a needle until it reaches the epidural space.
- Epidural is placed. Your anesthesiologist has to find the epidural space, most commonly through LOR or loss of resistance. This involves filling a needle with saline or air, applying constant pressure in the space, and feeling for when the pressure changes, indicating entrance into the epidural space.
- Catheter is threaded through the guidance hole; the needle is removed and the catheter is taped to your back.
- Release doses of anesthesia as needed, either by a healthcare professional or by the patient at their direction using a pump (with a dosage cap).
How are epidurals the same as spinal blocks?
Epidurals and spinal blocks both relieve pain using the spine, but the needs of each patient determine which solution is best. Around the spine is a dural sac of fluid; outside that is the epidural space. Spinal blocks are injected into the dural sac, and with this direct access comes a potent, fast-acting dose of whatever pain reliever is chosen. But that comes at the price of lasting only 1-2 hours. The length of a procedure or the degree of pain relief desired by the patient are the determining factors in choosing an epidural of spinal block.
How are epidurals different from spinal blocks?
Epidurals are pain relief tools, but they act on a completely different area of the spine: the epidural space. This is outside the central cavity of the spine, called the dural sac, so pain relief can’t reach the patient as quickly. However, after the 15-minute procedure and another 15-minute wait time, a healthcare professional or yourself can administer relief for as long as needed.
The biggest difference between epidurals and spinal blocks is how long they last and how much movement they permit. Epidurals last over ten hours and allow movement, while spinal blocks allow no movement and are short-lasting.
What is a walking epidural?
Most people can’t walk on an epidural, hence the name ‘walking epidural’ referring to the increased sensation left intact by this procedure. But this doesn’t mean there’s actually an epidural that permits walking around immediately following a procedure. These epidurals simply refer to greater mobility and feeling during and after the procedure. Many mothers now want to experience childbirth in a more involved manner.
- Less Medication: Epidurals include fentanyl or morphine to eliminate pain and epinephrine to keep blood pressure stable and extend the effect of the anesthetics. Walking epidurals simply use less of these medications. Pain is eliminated while preserving feeling and sensation to sit or lie, or push when the baby is ready.
Needles
Needles scare a lot of people, and nobody is excited when they have to get a shot. But epidural needles can be particularly scary. Images of huge needles being poked right into a spinal column would generally seem to be painful. Many women opt out of epidurals because they seem so unpleasant.
- Epidural catheter: The needles for epidurals are in fact large, because they insert a catheter in the epidural region. These catheters are the conduits for a variety of pain relief delivery options. The anesthesiologist or certified nurse practitioner will need to insert the needle and apply continuous pressure until they feel a change in resistance. The catheter is then inserted, and the needle withdrawn.
- Needle length: Averaging 8cm long, epidural needles have been known to frighten a lot of patients and attending spouses. However, the length is necessary to reach the epidural space via the lumbar region of the back. That the needle has gone far enough is obvious to the trained hands of the attending medical professional.
Pain
Don’t let literature on epidurals make you think that they’re not potent. This is an easy impression to get based on the idea that they allow semi-feeling and movement during procedures like C-sections. They can be just as potent as spinal blocks depending on the dosage, concentration of drug and the type of drug used. But when it comes to delivering children, they keep mothers semi-able to move the lower halves of their bodies.
- Local Anesthetics: These are applied to the area before the epidural needle is inserted. Doctors know that nobody likes pain—ideally 0—and they do their best to maximize pain reduction. A bit of pain and itching on part with a bug bite might result.
Side Effects of Epidurals
Epidurals affect the lower half of the body, so most of the potential side-effects are focused there. The important thing to keep in mind is to give your body time to recover, which it will do in just a few days.
Less medication is used during epidurals, but this does not mean you won’t have the same side effects. And anyone asking for less pain medication should be aware that in the event of peak pain, you will feel more of it. Particularly for first-time mothers, choosing between experiencing birth and experiencing an unknown level of pain, is challenging. In fact, many women decide on a classic epidural in the middle of birth, and it’s an easy switch for doctors to make.
- Sore Back: You may have pain around the injection site. This is common and short-term with most injections.
- Headache: This is a common post-anesethtic occurrence that will fade quickly.
- Blood pressure decrease: This happens as anesthetics vasodilate, but vasoconstictors are added to balance out blood pressure.
- Difficulty urinating: As your pelvic floor muscles regain feeling, this will become easier.
- Tingling or numbness
- Leg weakness
What Will an Epidural Feel Like?
There’s truly a wide range of responses to how epidurals feel. Some say bliss, some say extreme pain. Some women like to be in control of the timing, while some women report limited pain, despite successful epidurals. Sometimes the pain is isolated to one half of the body. But most women will feel no pain, although they will feel pressure at the site of their C-section, for example. Some women report the sensation of cutting but without any pain.
Safer Epidurals Using The Best Technology Available
Improve epidural efficiency and increase overall safety by trusting the latest technology. The CompuFlo Instrument is a tool that can help teams lower costs while maintaining precision and predictbaility throughout the procedure.
Detecting even the smallest of pressure changes right away so the patient avoids discomfort, CompuFlo lets you navigate the epidural needle with trust and confidence.
The CathCheck System is another valuable utility relied upon to confirm the exact placement of catheters in a matter of minutes.